Campaign: Snow Blow & Hiv
 Snow blow and HIV campaign resources
Snow blow and HIV campaign resources
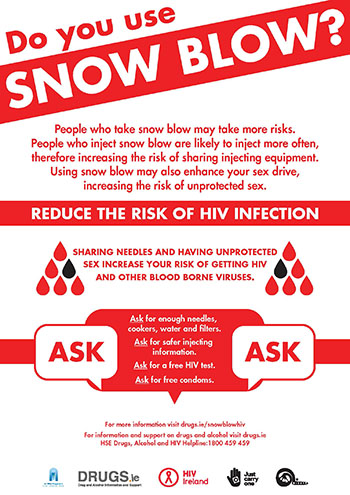
The ASK campaign is a harm reduction and HIV prevention campaign developed by Ana Liffey Drug Project & HIV Ireland.
The campaign aims to help address increasing HIV diagnoses among injecting snow blow users in Ireland.
Resources include:
- Snow blow Poster
- Snow blow fact sheet
- Snow blow booklet (print version is available from HIV Ireland & Ana Liffey Drug Project.)
Ask about snowblow
HIV diagnoses are increasing among people who inject the drug snow blow.
People might not always disclose that they are using snow blow.
For those working with people who currently use snow blow, remember to:
- ask if they are injecting snow blow or similar stimulants
- ask how many times a day they tend to inject snow blow
- ask if they have enough needles, cookers, filters and water
- ask if they want safer injecting information
- ask if they want free condoms
- ask if they would consider a free HIV test
What is Snow blow?
Snow blow is a type of drug called a cathinone. It is similar to cocaine in that it is a short-acting stimulant drug.
A number of different cathinones have been sold in Ireland as snow blow.
In powder form, cathinones are generally a fine white, off-white, yellowish or brown powder. They can also come in crystal form.
Cathinones can be snorted, injected, inhaled or taken orally.
Cathinone substances became well known in 2007 when they were available legally in head shops in Ireland and they continue to be used among certain drug-using groups in Ireland.
The Criminal Justice (Psychoactive Substances) Act 2010 effectively closed down the head shops by making it an offence to sell or supply for human consumption, substances which have psychoactive effects that are outside the remit of the Misuse of Drugs Act 1977.
However, many of these substances are now available through other channels and are still being used.
Between 2005 and 2014 more than 81 synthetic cathinone derivatives were reported to the European Union (EU) Early Warning System.
A number of cathinone derivatives have been sold in Ireland as snow blow, including:
- a-PVP
- MDPV
- butylone
- pentedron
- MDPBP.
What are the effects of snow blow?
Because snow blow is the name given to a number of different cathinone derivatives in Ireland, people may experience different effects depending on what cathinone they have taken.
Short-term effects of cathinones may include:
- elevated mood/euphoria
- increased confidence
- paranoia
- anxiety
- agitation
- aggression
- fits
- dehydration
- teeth grinding (Bruxism)
- increased blood pressure
- increased sex drive
- psychotic episodes
- hallucinations
- increased body temperature/hot flushes
- chest pain
- vomiting
- memory problems
- racing heartbeat/heart palpitations
- blue lips or limbs(from circulation)
- rapid rise in tolerance
- insomnia
- skin rashes
- decrease in appetite/weight loss
Does snow blow impact on mental health?
Snow blow use is associated with difficult comedowns and has also been associated with a recent increase in individuals presenting to emergency departments with acute psychotic episodes.
Of particular note is the suicide association with cathinones.
A UK study found a proportionally high-prevalence of cathinone drugs in hangings or other mechanical suicides (not suicide by drug overdose) compared to other new psychoactive substances.
Injecting Episodes
People who inject snow blow are likely to inject more often, therefore increasing the risk of sharing injecting equipment. Using snow blow may also enhance your sex drive, increasing the risk of unprotected sex.
Snow blow is a short-acting stimulant type drug similar to cocaine or amphetamines - meaning people tend to re-dose frequently - with some reporting injecting between 10-20 times a day.
This can result in users running out of clean injecting equipment and reusing or sharing equipment.
Snow blow users should be encouraged to ask for enough needles, cookers, filters, water, injecting information and condoms at their needle exchange.
Overdose
It is possible to overdose on stimulant drugs.
Signs of an overdose are:
- overheating
- blue lips or limbs
- fast breathing or difficulty breathing
- rapid heartbeat
- seizures
- shaking
- paranoia
- psychosis
- loss of consciousness.
If you encounter someone who has overdosed on snow blow, place them in the recovery position and call 112.
Snow blow and HIV
In February 2015, an outbreak of recently acquired HIV infections among people who inject drugs (PWID) was identified in Dublin.
A multidisciplinary incident team was set up by the Director of Public Health in Dublin to investigate and respond to the increase.
Clinicians were concerned that the increase was linked to injection of the synthetic cathinone a-PVP, street name snow blow, with more frequent injecting and unsafe sexual and needle-sharing practices.
The increases were mainly seen in chaotic polydrug users, many of whom were homeless.
An epidemiological investigation and case-control study were undertaken by the HSE which reported the following summary results:
- in 2014 and 2015, 38 confirmed and probable cases of HIV were reported
- among these, 16 were female
- 29 of the 38 had been registered with homeless accommodation services
- all females and 13 of the 20 males with information available were homeless
- 18 of the 20 PWID with information available reported injecting snow blow
- at risk practices, namely sex with PWID, or sex with an HIV-positive partner were reported by 20 of the 38 cases
- 13 cases reported both using snow blow and sexual at-risk practices
- the odds of recent HIV infection was highest in those who reported injecting snow blow daily
The investigation is the first evidence of an association between injecting snow blow and recent HIV infection in Ireland, with daily snow blow injectors being at highest risk.
Snow blow has been found to contain a-PVP, a second generation cathinone and is closely related to MDPV.
Report on the epidemiological investigation and case-control study
In Dublin, there are more than 500 homeless PWID, a significant population at risk of HIV infection. For those working with PWID who may be at risk, there are a number of measures that can be taken:
- encourage HIV-positive PWID to engage in HIV care
- encourage PWID to get tested for HIV - it’s free at a range of clinics
- raise awareness about the risks associated with injecting head shop drugs such as snow blow, including sexual at risk behaviours, and provide harm reduction information
- encourage PWID to engage with methadone and treatment services
Safer Injecting and snow blow
Snow blow users tend to inject more often, therefore they require more injecting equipment. It is helpful to ask how many times a day they expect to inject - and to then calculate how much equipment they will need.
Harm reduction advice for safer injecting:
- always divide your snow blow before you begin injecting if using with a friend or group
- start low and go slow - always start with a small test dose to see how you react to the drug and inject slowly
- cook up with clean sterile water. Substances should be fully dissolved before injecting - citric may not be needed
- don’t reuse the same needle. Needles become blunt after being used once. If you don’t hit a vein the first time, use a new needle until you inject successfully
- snow blow injectors often experience a painful burning sensation, swelling and discomfort at injecting sites. Snow blow injecting can leave wounds which take some time to heal. Place a plaster over these sites and try to not use them to inject
- always rotate injecting sites
- avoid using snow blow with other drugs including alcohol and prescription medication
- use your own injecting equipment. Sharing injecting equipment increases the risk of getting blood-borne viruses like HIV
- stay hydrated and try to drink a pint of water an hour
- use in trusted company, never use alone
- it can be hard to inject snow blow without causing pain and soft tissue damage. Improving injecting technique can reduce discomfort, vein damage and the risk of getting blood-borne viruses. Safer injecting advice is available from needle exchange services
- when injecting snow blow the urge to share needles is usually strongest after you have used. Snow blow can make people feel close or connected to the people they are injecting with. These feelings could lead to sharing snow blow or sharing equipment.
Safer Snorting
Snorting snow blow is generally less harmful than injecting.
Harm reduction advice for safer snorting:
- grind snow blow before snorting as it may have crystals or clumps in it
- place the tooter high up the nostril to avoid damaging the bottom of the nose
- use your own tooter. Sharing tooters increases the risk of spreading blood-borne viruses like HIV
- bank notes are more likely to contain germs or traces of blood from other people. It is safer to use a clean straw cut in half or some rolled up cardboard
- alternate nostrils to give each side a break
Safer Sex
Condoms, when used consistently and correctly, are the best way to prevent the sexual transmission of HIV and other sexually transmitted infections (STIs).
Using snow blow can increase a person’s sex drive, therefore increasing the risk of unprotected sex. Encourage service users to be prepared and carry condoms with them.
Condoms are available for free in all needle exchanges. Encourage service users to ask for free condoms at their needle exchange.
A list of organisations that provide free condoms.
Safer Sex Advice for people who use snow blow:
- ask for free condoms at your needle exchange
- carry condoms with you at all times, particularly when you know you will be using snow blow
- use condoms every time you have sex
- only use a condom once. Never re-use it!
- get tested regularly for HIV and other STIs. Testing is free in public clinics
Information on condoms and how to use condoms correctly
HIV Testing
People can have HIV and not have any symptoms.
The only way to know if a person has contracted HIV is to get tested.
By getting tested and knowing your HIV status you can:
- get the essential care necessary for living a healthy life with HIV
- make informed decisions about preventing transmission of HIV
- protect your partner(s) as well as yourself
HIV testing is confidential. Pre and post-test counselling may be available at some testing clinics.
HIV testing is available free in Ireland at public testing clinics. The HIV test is a blood test.
Information on HIV transmission, prevention, testing and treatment.
PEP (post exposure prophylaxis)
- PEP is a course of medication that aims to prevent HIV infection following a recent sexual or needle-stick exposure to HIV. PEP works to prevent HIV from establishing itself in the bloodstream
- PEP must be taken within 72 hours (3 days) after the possible exposure to HIV, and sooner if possible
- PEP is effective but is not a cure for HIV
- PEP is only available by prescription from some hospital emergency departments and HIV/STI clinics. Not everyone will be prescribed PEP – this is based on an assessment at the clinic or hospital
Anyone who discloses a potential recent exposure to HIV, through unprotected sex or from a needle, should be referred to a hospital emergency department or HIV/STI clinic to get assessed for PEP. Ensure that the potential exposure was within the 72 hour time period before referring as PEP will not be prescribed once this time has elapsed.
More Information and Services
HIV Ireland
www.hivireland.ie
Free HIV and STI testing on the second and fourth Wednesdays of every month. Free condoms – walk-in service. Free community support services for people living with HIV. List of other free HIV testing clinics and services. List of other organisations where free condoms are available. List of clinics and hospitals that provide PEP. A range of downloadable resources on HIV and sexual health.
Drugs.ie Services Directory
www.drugs.ie/services
List of Needle Exchanges. List of Drug and Alcohol Services. A range of downloadable resources. Online Chat Service.
Ana Liffey Drug Project
www.aldp.ie
Open Access Service. Needle and Syringe Outreach Programme. Medical Services. Case Management Service.
HSE Helpline
Freephone:1800 459 459
Drugs, Alcohol, HIV, Hepatitis and Sexual Health Helpline.